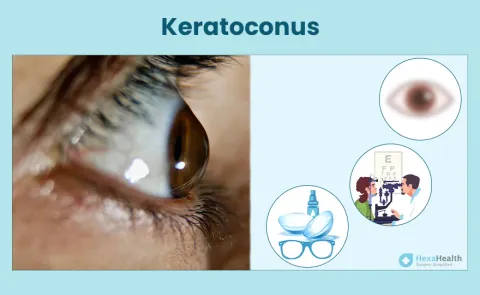
Risks in Delaying Treatment of Keratoconus
If left untreated, keratoconus progresses over time, leading to several side effects. In some rare cases, untreated keratoconus can even result in permanent vision loss. Other side effects include corneal scarring, making it difficult to wear contact lenses and leading to emotional distress.
Stages of Keratoconus
Progression of keratoconus occurs differently in each eye. If the condition develops at an early age, the progression is generally more rapid. The disease's most rapid and significant progression occurs within the first 15-20 years after onset.
Early Keratoconus
There is only a slight corneal distortion in this stage, having little or no effect on the quality of vision. Doctors usually recommend spectacles to correct myopia and astigmatism and provide adequate vision.
Moderate Keratoconus
In this stage, the corneal distortion increases, and the change in the shape of the cornea can be observed. The vision quality decreases with spectacles, and rigid gas permeable contact lenses become a better choice.
Advanced Keratoconus
There is a slight to moderate scarring of the cornea and a substantial corneal distortion in this stage. To maintain the appropriate fitting, you may require rigid gas permeable contact lenses with steeper inside curvatures.
Severe Keratoconus
In this final stage of keratoconus, the corneal distortion is dramatic, along with substantial corneal scarring and thinning. You may need to consult an experienced corneal surgeon for a corneal transplant at this stage.